For most people, varicose veins aren't cause for alarm. But advanced cases may cause pain or indicate a more serious health concern.
Varicose veins are very common – about 1/3 of all adults have them. If you have Medicare and are suffering from symptoms of varicose veins, you may be wondering if Medicare covers any treatment.
Medicare Part B does cover some varicose vein treatments if certain conditions are met. Read on to learn more about what varicose veins are, including symptoms and causes, when they need treatment and what treatment options are available, Medicare’s coverage for treatment, and how much treatment will cost.
What are varicose veins?
Varicose veins are swollen, twisted, blue or purple bulges just under your skin’s surface, typically appearing in your legs, feet, and ankles. (Spider veins, which are smaller red or purple lines that appear close to your skin’s surface, may surround varicose veins.)
When the walls of your veins weaken and blood pressure in your vein increases, the weakened walls allow your vein to get bigger. As it stretches, the valves that keep blood moving don’t work like they should, and slow blood backs up or pools in your vein. This causes the vein to swell, bulge, and twist.
While they can be unsightly and uncomfortable, varicose veins aren’t dangerous for most people.
Symptoms of varicose veins
Varicose veins typically develop in clusters and may be itchy, painful, or sore. Your legs, ankles, and feet may swell and throb, or muscles in your legs may feel tired, heavy, or sluggish. If left untreated, varicose veins can also cause brown discolorations on your skin.
Causes of varicose veins
Anyone can develop varicose veins but they become more common as you age. Veins lose elasticity and stiffen over time, so the vein walls and valves don’t work as well as they once did.
Female hormones can also allow the walls of the veins to stretch, so some women are at higher risk.
Lifestyle, such as standing or sitting for long periods or wearing restrictive clothing, and some health conditions, can increase the pressure in the veins or decrease circulation and blood flow, leading to varicose veins. Smokers and those with a family history of varicose veins are also at higher risk.
When do varicose veins need treatment?
In some cases, severe varicose veins can lead to health problems such as blood clots. They can also cause venous ulcers, or sores, on your skin.
Additionally, severe varicose veins may be a sign of chronic venous insufficiency, which is a condition that affects your veins’ ability to pump blood to your heart.
If you have varicose veins, tell your primary care provider. They can evaluate and monitor you for any severe symptoms and recommend the best treatment options for you.
Varicose vein treatment options
There is no cure for varicose veins, but there are some treatments that can reduce their appearance and relieve any discomfort. For example, to increase blood flow and decrease pressure, elevate your legs above your waist multiple times per day. You can also wear supportive stockings or socks.
Another treatment option is called sclerotherapy, or injection therapy. During this treatment, your doctor will inject a solution into your vein that causes the walls to stick together, and eventually the vein will turn to scare tissue and fade away.
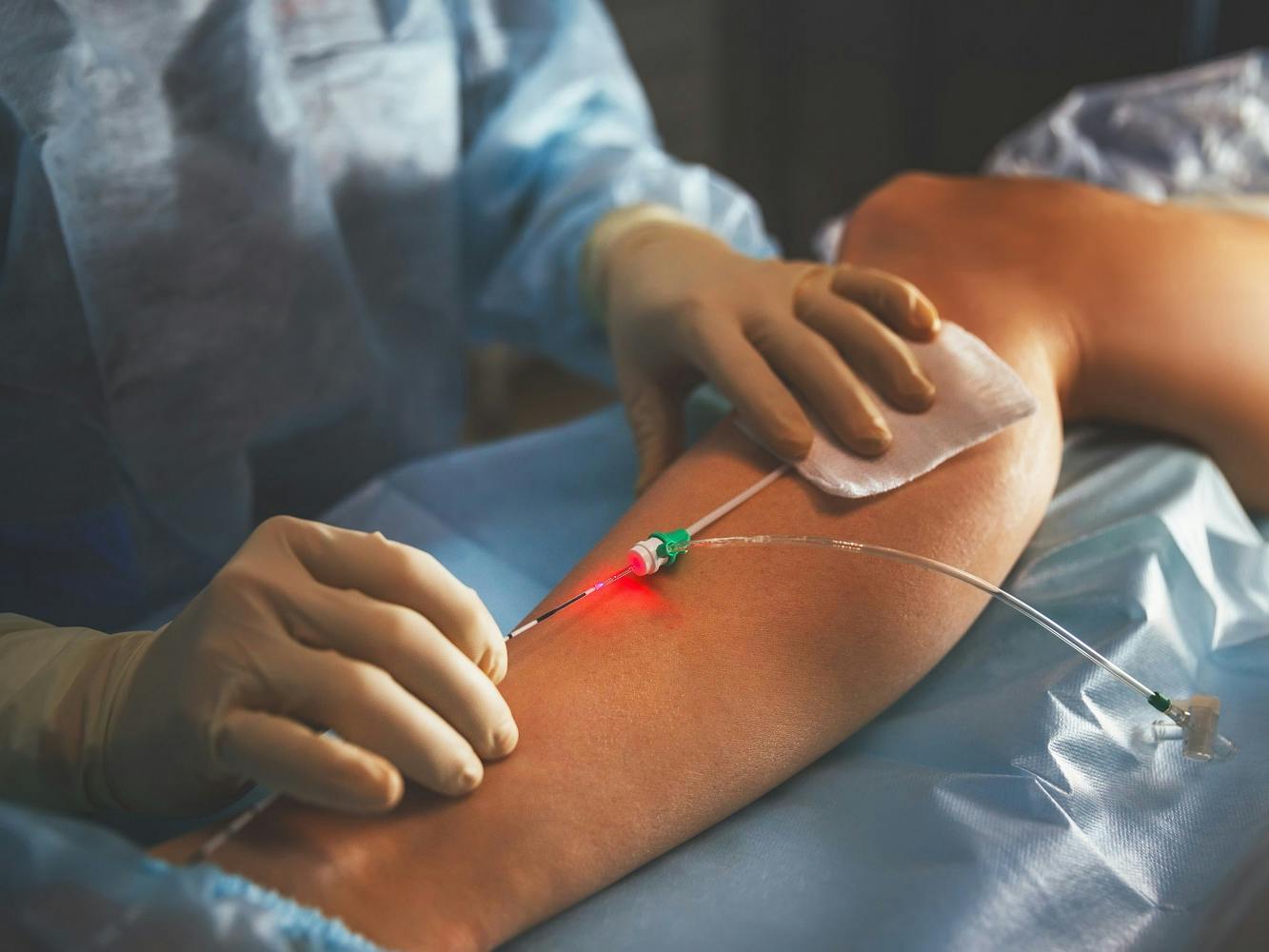
Laser therapy is another option. Called endovenous thermal ablation, this is minimally invasive procedure where a doctor uses a catheter and laser to close off a damaged vein. Or, your provider may recommend VenaSeal, which is a medical-grade glue that’s placed inside a varicose vein using a tiny catheter, sealing the vein wall together.
In severe cases, your doctor may recommend surgery. During these procedures, called ligation and stripping, the surgeon will tie off your affected vein to stop blood from pooling and remove the vein to prevent reappearance.
Medicare coverage for varicose vein treatment
Medicare will cover varicose vein treatment if it’s considered medically necessary. Medical necessity is determined by your provider and may be considered if you experience common varicose vein symptoms, bleeding from the veins, related blood clots, ulcers, or other reasons.
In most cases, patients must first try conservative treatment, such as elevation, exercise, weight loss, and compression stockings, for up to 12 weeks without good results.
If deemed medically necessary, Medicare Part B (medical insurance) will cover treatments like sclerotherapy (or micro sclerotherapy), endovenous ablation therapy, endoscopic vein surgery, or laser vein surgery.
How much will varicose vein treatment cost?
If your treatment is covered by Medicare, you must first meet the Part B deductible ($226 in 2023). Then, you will be responsible for 20% of the Medicare-approved cost. Medicare will pay the remaining 80%.
If you have a Medicare Advantage plan your costs may be different, so check with your insurance plan for more information. If you have a Medigap plan, it may help pay for your deductible and coinsurance costs.
Comparing Medicare plans is easy with our Find a Plan tool. Just enter your zip code to review the costs and benefits of Medicare plans in your area, including Medicare Advantage, Medigap, and Part D prescription drug plans. Or, call us toll-free at 888-992-0738 and one of our licensed agents will answer your questions and help you choose the right Medicare plan for your unique needs and budget.
Additional resources
- ClearMatch Medicare: Find a Medicare Plan
- Cleveland Clinic: Varicose Veins



